Part of a successful non surgical treatment
for children and adults
What is Neuromuscular Scoliosis?
Muscular Dystrophy and Scoliosis
Neuromuscular Scoliosis Treatments
Bracing for Neuromuscular Scoliosis
Neuromuscular Scoliosis Surgery
What is Neuromuscular Scoliosis?
Scoliosis is a term used to describe any abnormal curvature in the spine or backbone. There are many types of scoliosis and corresponding causes. A structural scoliosis is a fixed curve (as opposed to a reversible or “nonstructural” curve). This type of scoliosis can be caused by:
- Birth defects (such as misshapen spinal bones formed before birth)
- Injury to the spine, pelvis, or legs
- Infections of the spinal bones
- Tumors of the spine
- Metabolic diseases
- Connective tissue disorders
- Arthritis
- Unknown factors (idiopathic scoliosis, the most common type of scoliosis)
- *Neuromuscular diseases
Neuromuscular Scoliosis
Neuromuscular scoliosis is caused by a problem with the nerves and muscles of the body. The most common symptom of neuromuscular diseases is therefore muscle weakness. Neuromuscular scoliosis can also develop in individuals due to birth defects or conditions such as: muscular dystrophy, cerebral palsy, or spina bifida. Patients with these conditions typically develop a long “C” shaped spinal curvature because their muscles are unable to hold their spine straight.
Cerebral Palsy and Scoliosis
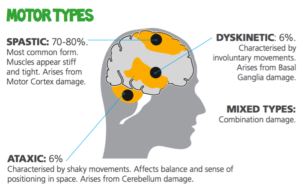
Cerebral palsy is a group of disorders that leads to weakness in the abdominal and spinal muscles effecting posture which can cause spinal deformities.
There are several different types of cerebral palsy, including:
- Spastic
- Dyskinetic
- Ataxic
- Hypotonic
- Mixed
Spinal deformity is a common musculoskeletal problem only for individuals with specific types of cerebral palsy. Scoliosis frequently occurs in patients who have spastic cerebral palsy or hypertonic cerebral palsy. Spastic CP is a form of cerebral palsy in which tightness, stiffness, and/or pull of muscles is either the main or only impairment. It is the most common type of cerebral palsy and occurs in 90% of all cases. Hypertonic CP is considered a variant of spastic CP but also features extremely stiff muscles. It accounts for 80% of all cases in the US.
Scoliosis in cerebral palsy patients differs from idiopathic scoliosis in that the curve is a typically long and c-shaped curve. A long single thoracolumbar curve is the main scoliosis pattern of spastic cerebral palsy patients. In many cases, even after these patients have finished growing, their curvature will continue to get larger. Severe cerebral palsy scoliosis can impair physical function and cause pain and balance problems for patients who are wheelchair dependent. These patients often have breathing and heart problems as well.
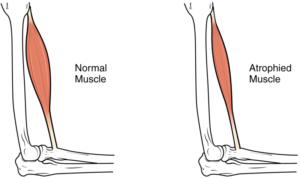
Muscular Dystrophy and Scoliosis
Muscular dystrophy or “MS”, is a group of diseases that cause progressive weakness and loss of muscle mass. In muscular dystrophy, mutated genes affect the production of proteins needed to form healthy muscle. Scoliosis is a common problem in patients with muscular dystrophy. The scoliosis develops early and tends to be rapidly progressive, especially in non-ambulatory patients (those who cannot walk). The scoliosis is typically thoracolumbar (in the mid and lower spine) or lumbar (lower spine) with associated pelvic obliquity (tilted pelvis), thoracic kyphosis (hunch back), and lumbar hyperlordosis (swayback)
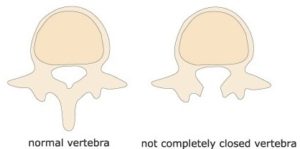
Spina Bifida and Scoliosis
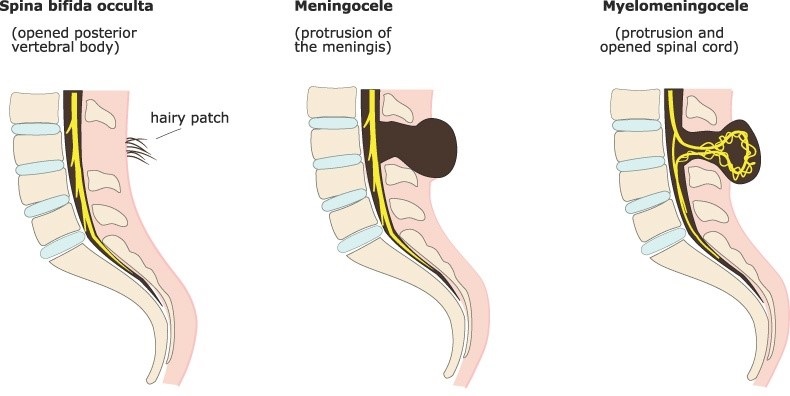
Spina bifida is a birth defect in which there is incomplete closing of the spine and membranes around the spinal cord during early development in pregnancy. There are three main types: spina bifida occulta, meningocele and myelomeningocele.
Myelomeningocele also known as open spina bifida, is the most severe form. It can be associated with severe disability including: poor ability to walk, problems with bladder or bowel control, accumulation of fluid in the brain (hydrocephalus), tethered spinal cord (when the spinal cord is attached to tissue around the spine and cannot move freely within the spinal canal). In some individuals, this causes significant traction and stress on the spinal cord and can lead to a worsening of associated paralysis, scoliosis, and back pain.
Bracing for Neuromuscular Scoliosis

Some patients with neuromuscular scoliosis can be effectively treated with bracing. While bracing can not correct this type of scoliosis, an innovative brace design called “suspension bracing” can be very helpful in those patients who have enough balance and core strength to sit unassisted. This brace option is particularly beneficial for those patients who reject the surgical option. Patients reject surgery for a variety of reasons, such as having other health problems that make general anesthesia dangerous or religious beliefs against blood transfusion (Jehova’s Witnesses).

The Suspension Trunk Orthosis (STO) scoliosis brace prescribed for neuromuscular scoliosis is similar to a Thoraco-Lumbo-Sacral Orthosis (TLSO) scoliosis brace, except it does not rest against the patient’s pelvis but directly against the seat. The STO brace relieves the pressure placed on the lower abdomen by the weight of the upper body. The brace also relieves the over-pressure on the buttocks from the seat. By reducing this abdominal pressure, patients are able to use their diaphragm more effectively and breath more deeply and fully with less exertion. A further benefit of suspension bracing is that it stabilizes the shoulders to allow better use of patient’s arms.
| Neuromuscular scoliosis progression is different from that of idiopathic. Once the scoliosis appears, the curve tends to get worse. Therefore, prescribing a corrective orthosis is of great benefit, even in small curve sizes. |

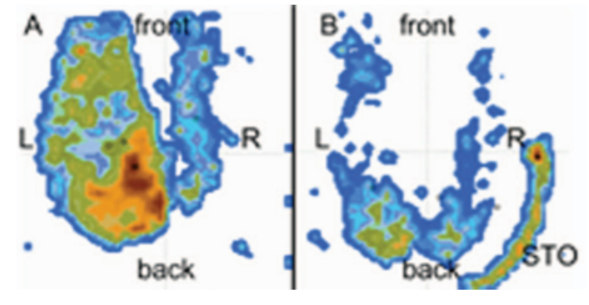
When patients aren’t in the brace, all of their body weight is pushing into the seat through their lower pelvis, mostly the area of the ischial tuberosities or what are commonly called “sit bones”. Prolonged pressure and reduced activity due to weak muscles may result in severely reduced blood circulation in these areas. If they already have a pelvic asymmetry that causes them to lean to one side, this one-sided pressure can make the spinal curvature worse. A suspension brace changes the distribution of weight and pressure on the body. The body weight is partly supported by the upper part of the brace just below the shoulders, by the unique design. The brace has a tulip shape that keeps the patient upright in the brace. The figure below shows the drastic decrease in pressure on the buttocks, comparing to the un-braced sitting position. This greatly reduces the risk of developing pressure sores.
The bottom of the pelvic bones touch the seat of the wheelchair and so do the backs of both thighs. Adjustments to the brace are sometimes necessary to achieve the correct weight transmission and take pressure off the thighs and buttocks. The final length of the brace is established after careful fitting.
Advantages of sitting in a suspension brace:
- Decompression of the fragile soft tissue, preventing pressure sores
- Control of weight and pressure transmitted by the lower portion of the brace
- Creating a stable foundation for the patient’s shoulders and arms
Neuromuscular scoliosis patients typically have poor sitting balance and have only a few sitting positions that are stable. Patients may be afraid to fall forwards, backwards or to one side. These issues are carefully managed with appropriate fitting. We use an advanced molded form of the lower section of the orthosis, which pushes from the back in order to maintain and support the normal shape of the lower spine.
The suspension brace is usually well tolerated and patients are able to spend from 3-6 hours each day in the brace, however, the movement is obviously limited during this time. The brace allows patients previously unable to sit to do so, improvement to those with poor sitting balance and alleviates pressure pain in the pelvic region from the wheelchair.
Myelomeningocele patients often need a period of adaptation to the new trunk elongation position, which causes a much higher head level. Breathing is uninhibited due to the tulip shape of the thoracic part of the brace. Patients report improvement of respiration in brace.
The benefits of suspension bracing used for progressive neuromuscular scoliosis are all about improving the Quality of Life:
- Improve sitting or allow for sitting in selected non-sitting patients
- Dramatically slow or even stop the progression of the scoliosis
- Improve pelvic obliquity/asymmetry (sideways tilt)
- Significantly reduce pressure on the internal organs, specifically the digestive organs and the lungs
- Reduce pressure on buttocks and thighs
- Provide better strength and freedom of movement of the arms and shoulders
- Increase daily hours spent in a functional position
- Delay surgery (in cooperation with the surgeons planning)
- Reduce the extent of surgery (anterior spinal procedure may be spared, if the size of the scoliosis angle is controlled with the brace).
|
Brace treatment can slow the progression of the curve, delay surgery, improve the function of sitting and use of arms and decompress the abdomen. |
Regular office visits are necessary to monitor for any issue that may require modifications to the brace (such as skin irritation, imbalances, unstable sitting, or pain). Patients receive a brochure with instructions for home care of the brace and proper use.
If you are considering scoliosis bracing for neuromuscular scoliosis, please contact our office for a free consultation.
Email: info@hudsonvalleyscoliosis.com
Call: +1 (845) 620-0010
Surgery for Neuromuscular Scoliosis
Surgery may be necessary for patients suffering from neuromuscular scoliosis. Instrumentation and fusion of the whole thoracic (mid) and lumbar (lower) spine with pelvis fixation to correct pelvic obliquity (tilt) is the most common recommended.
When is Surgery Necessary?
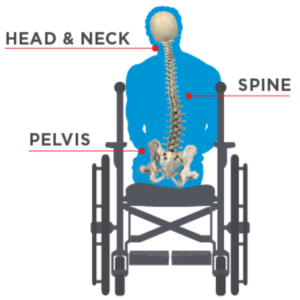
Scoliosis surgery may be recommended for cerebral palsy patients, as spinal fusion can (in some cases) produce a stable torso that improves sitting and orienting. Cerebral palsy patients attempting to walk sometimes seek surgical correction to improve their balance and walking ability. However, the process of surgery is strenuous and the results can be affected by significant complications. Because the pelvis and the spine are connected, any surgical procedures to correct cerebral palsy scoliosis should take into account the possibility of a misaligned pelvis. In patients with significant pelvic twisting (a common condition of the pelvis in CP) or who are at risk of developing pelvic twisting, metal rods and screws extend to the pelvis, particularly in children who are unable to walk.
The age when surgery is recommended typically depends on the level of deterioration of the main scoliosis curve. Most patients receive surgery in early adolescence, however surgery may be safely performed in adult patients. In severe neuromuscular scoliosis, an additional stage of scoliosis surgery is sometimes necessary. Thus, successfully controlling the scoliosis curve with a scoliosis brace may prevent this second stage of surgery.
It has been suggested that spastic cerebral palsy patients with certain risk factors for progressive scoliosis might benefit from early surgical intervention to prevent progression of their scoliosis, but not all patients or their families make this choice.
Most research approves of surgical treatment for spastic scoliosis, however there are differing views on when surgery is necessary. Miller recommends posterior spinal fusion and unit rod fixation for all flexible scoliosis curves between 45° and 90° in children older than 15 years and for correctable curves of less than 90° in children older than seven. For curves larger than 90°, he suggests combining the procedures with anterior spinal release. Children younger than seven with curves around 60° are on the borderline.
When Should Surgery be Avoided?
There are many situations when surgery cannot be offered or needs to be postponed (certain blood disorders, anesthetic concerns, parents’ refusal). Kennedy et al. reported that in patients with Duchenne muscular dystrophy, spinal surgery consisting of posterior stabilization improved sitting function and facilitated nursing care, however it did not alter the inevitable decline in lung function. These patients still experienced deterioration of lung function of 3 – 5% per year.
If patients suffer from breathing issues, anesthetic used during surgery may pose significant risks. For severe curvatures, the additional anterior fusion/instrumentation may cause increased impairment of respiratory function. Successful control of the curve with a brace may help to prevent the anterior stage of spinal surgery.
What are the Risks of Surgery?
Much of the research stresses the high risk of complications of these extensive surgical procedures with the frequency of postoperative complications between 8% and 47%.
Most common complications:
- Urinary tract infections
- Cardiopulmonary issues
- Gastrointestinal complications
- Behavioral problems
- Skin healing problems
Late complications include:
- Delay or lack of spinal fusion
- Loss of correction,
- Instrumentation damage
- Heterotopic ossification (abnormal growth of bone in the non-skeletal tissues including muscle, tendons or other soft tissue)
Surgical treatment cannot be avoided in most cases of progressive neuromuscular scoliosis, however there is a definite place for conservative scoliosis treatment, consisting of physical therapies, exercises, and innovative conservative management of neuromuscular scoliosis suspension bracing. Brace treatment is able to prevent the collapse of the abdomen, improve the sitting position and take pressure off the body’s organs.
Neuromuscular scoliosis is an extremely complex condition best treated with a team approach. Continuously improving techniques of conservative scoliosis treatments, such as bracing, exercises, and scoliosis specific therapies, together with appropriately timed surgery provides the optimal treatment program for patients.
Source
Kotwicki, M. Jozwiak, Conservative management of neuromuscular scoliosis: personal experience and review of literature, Disabil. Rehabil. 30 (2008) 792–798